The liver is a vital organ in a child’s overall well-being—aiding digestion, detoxifying toxic substances, synthesizing essential proteins, and storing energy. But like any other organ, it can be influenced by disease. Liver diseases in children are generally divided into two categories: congenital and acquired. Knowing the difference between the two is important for early detection, successful treatment, and supportive therapy.
What Are Congenital Liver Diseases?
Congenital liver diseases are diseases that an infant is born with. These usually result from genetic defects, pregnancy complications during development, or issues with liver or bile duct formation.
Common Congenital Liver Diseases
- Biliary Atresia
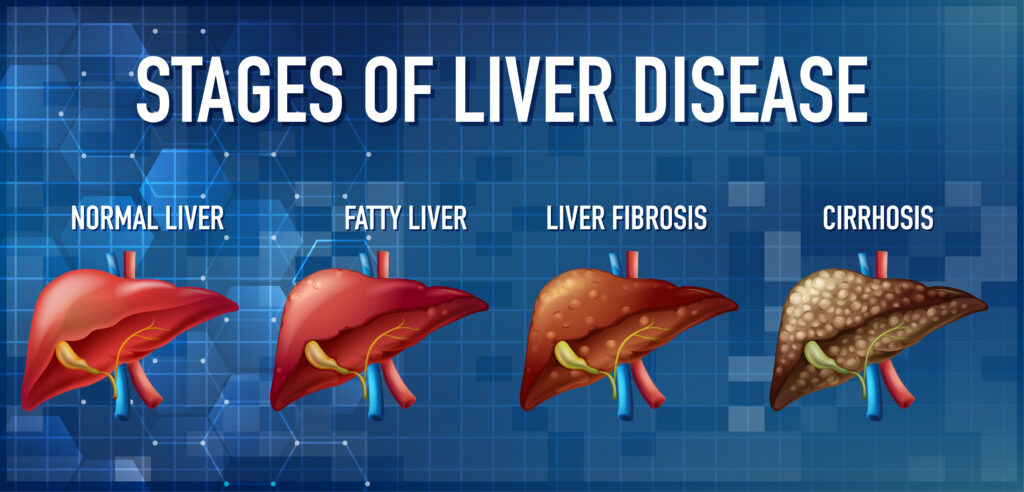
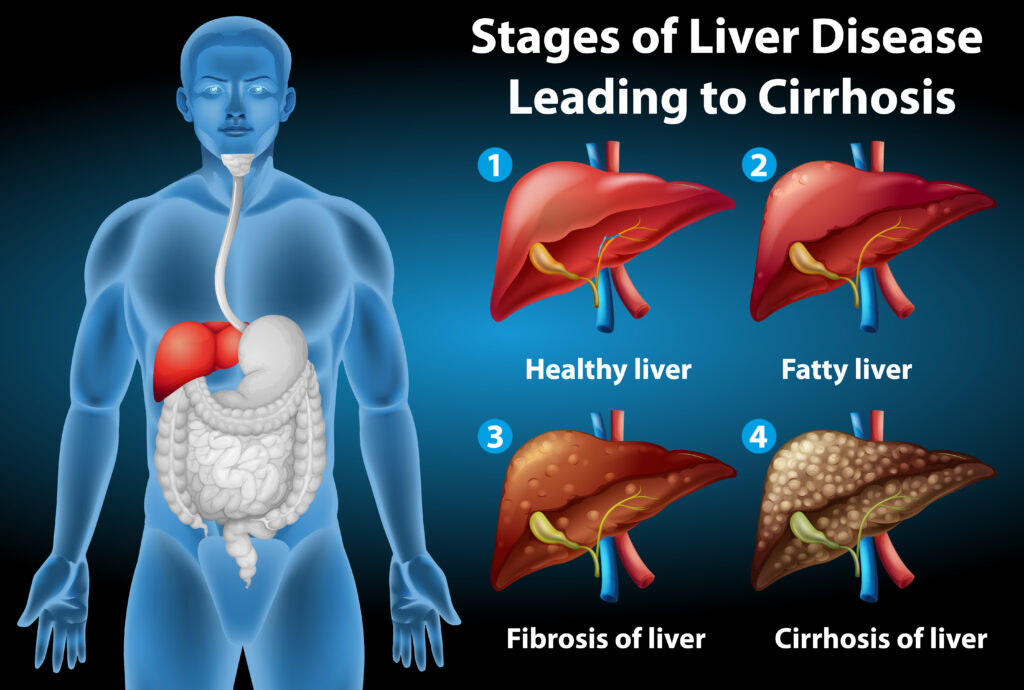
A rare but serious illness in which the bile ducts are either missing or blocked, so that bile cannot flow from the liver into the intestine. This causes liver damage and scarring.
- Alagille Syndrome
A genetic disorder of the liver, heart, and other systems. It is associated with underdeveloped bile ducts and jaundice and liver fibrosis.
- Alpha-1 Antitrypsin Deficiency
A genetic disorder that makes the body produce defective alpha-1 antitrypsin protein, which may build up in the liver and cause damage.
- Cystic Fibrosis-Related Liver Disease
In children with cystic fibrosis, thick mucus may clog bile ducts, resulting in liver problems.
What Are Acquired Liver Diseases?
Acquired liver diseases are diseases that occur after birth, most commonly as a result of infections, environmental exposures, autoimmune reactions, or habits.
Common Acquired Liver Diseases in Children
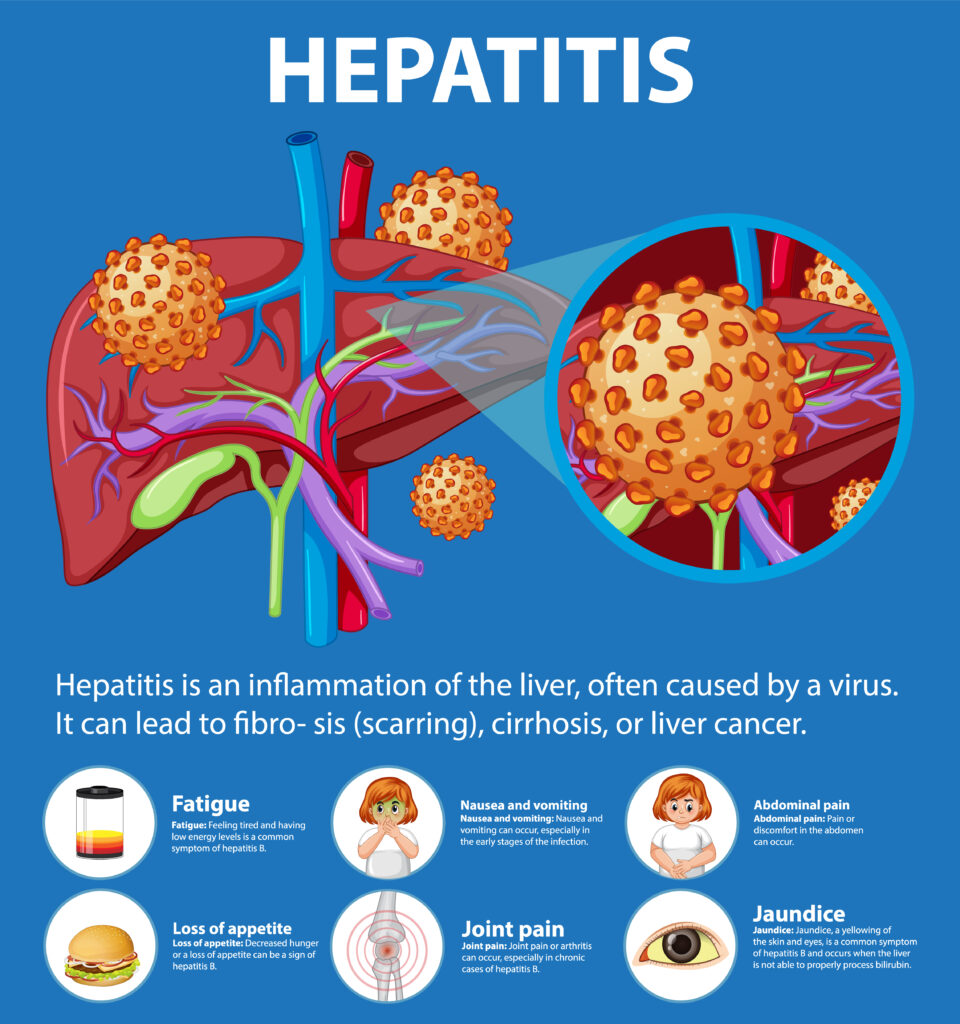
- Hepatitis A, B, and C
Viral infections that result in inflammation of the liver. Hepatitis A is typically transient, whereas B and C may result in chronic diseases.
Increasingly common due to rising obesity rates in children. It involves fat buildup in liver cells and can progress to liver damage.
- Autoimmune Hepatitis
A condition where the immune system attacks liver cells, causing inflammation. It can lead to scarring and liver failure if not treated.
- Drug-Induced Liver Injury
Certain medications or supplements can be toxic to the liver, especially if used inappropriately or for extended periods.
Key Differences Between Congenital and Acquired Liver Diseases
| Timing of Onset | Present at birth | Develops after birth |
| Causes | Genetic, structural defects, prenatal factors | Infections, autoimmune responses, lifestyle |
| Diagnosis | Often within the first few months of life | May appear in infancy, childhood, or adolescence |
| Examples | Biliary atresia, Alagille syndrome | Hepatitis, NAFLD, autoimmune hepatitis |
| Treatment Approach | Often surgical or transplant-based | May include medication, lifestyle changes, or antiviral therapies |
Signs and Symptoms to Watch For in Both Types
Although causes vary, most liver diseases in children have the same symptoms:
- Jaundice (yellowing of eyes/skin)
- Dark urine and pale stools
- Poor weight gain or growth
- Swollen belly (ascites)
- Itching and irritability
- Fatigue and loss of appetite
Early detection and medical consultation are essential to avoid complications.
Diagnosis and Treatment
Diagnosis
- Blood tests: Liver function tests, genetic screening, autoimmune markers.
- Imaging: Ultrasound, MRI, or CT scan to assess liver structure.
- Liver biopsy: In a few instances, a tiny liver tissue sample is studied.
Treatment Options
- Congenital Diseases: Surgery (e.g., Kasai procedure for biliary atresia), enzyme replacement, or liver transplant may be needed.
- Acquired Diseases: Treated with medications (antivirals, immunosuppressants), diet modification, or treatment of underlying infections.
Living With Liver Disease: Supporting Children and Families
Living with a chronic liver disease can be physically and emotionally challenging—both for the child and family. The help of pediatric liver experts, nutritionists, therapists, and support groups can make a significant difference. Children with liver disease can have satisfying lives with proper care and early treatment.
Frequently Asked Questions (FAQs)
1. Can congenital liver diseases be prevented?
Most congenital liver diseases can’t be prevented since they are developmental or genetic in origin. Prenatal screening and genetic counseling can, however, help evaluate risks.
2. Is liver disease in children curable?
Certain diseases of the liver can be controlled or even cured, particularly if diagnosed early. Others, especially the genetic and autoimmune diseases, might need a lifetime regimen or even transplantation.
3. How common is liver disease in children?
Liver illness in children is not very common in comparison to adults, yet occurrences—particularly of fatty liver disease—are increasing with obesity and metabolic syndrome.
4. How is the outlook for children with liver illness?
Through early diagnosis and proper treatment, most children recover or control their illness well. Liver transplants are very successful when necessary.
5. What are indications that my child may require a liver transplant?
Symptoms are liver failure symptoms (jaundice, edema, bleeding disorders), growth failure, tiredness, and declining lab values. A transplant team will assess based on several variables.
Final Thoughts
Whether congenital or acquired, liver disease in children requires a proactive approach involving early detection, medical management, and ongoing support. Understanding the differences between these types not only helps caregivers advocate for timely care but also empowers them to offer the best support to their children. If you suspect liver-related issues in your child, don’t hesitate to consult a pediatric gastroenterologist or hepatologist.